Beyond LDL: The TG/HDL Ratio as a Game-Changer in Heart Health
Why this often-overlooked ratio could redefine cardiovascular risk assessment and help prevent heart disease—even in those with ‘safe’ LDL levels
When we receive our annual lipid panel results, the focus is often on LDL-C, the so-called “bad” cholesterol, with high numbers prompting a quick recommendation for statins. We might give HDL-C, the “good” cholesterol, and triglycerides a quick look, just to see if they fall within the recommended range. But this quick glance could be a mistake. Digging deeper into these numbers reveals a key insight: the Triglyceride-to-HDL-C (TG/HDL-C) ratio might actually be one of the most important markers for cardiovascular risk. By paying closer attention to this ratio, we could significantly improve our understanding of heart health and possibly prevent adverse cardiovascular events.
The TG/HDL-C ratio has emerged as a valuable biomarker for cardiovascular health due to its strong associations with several key cardiovascular risk factors and outcomes. Dr. Robert Lustig (who authored the must-read book, Metabolical), emphasizes the importance of the triglyceride to HDL ratio as a crucial marker of metabolic health. He suggests that this ratio is more informative than looking at total cholesterol or isolated LDL numbers alone. He advises prioritizing this ratio over other lipid markers, suggesting that people should strive to maintain triglycerides below 100 and HDL levels above 60 for a healthier lipid profile. Lustig's focus on this ratio indicates that he considers it a more valuable metric than LDL-C numbers in assessing overall metabolic health and cardiovascular risk. Lustig recommends aiming for a triglyceride to HDL ratio below 1.5 for optimal health.
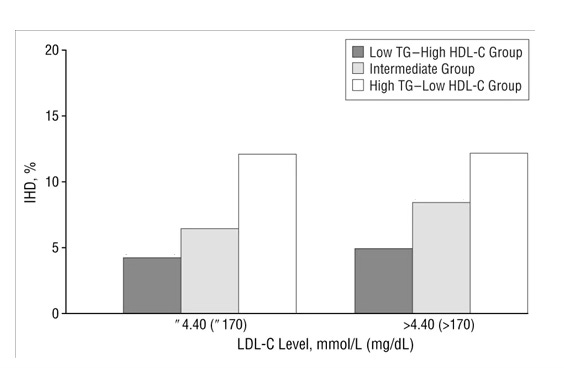
A study published in JAMA Internal Medicine found that men with high LDL-C but low TG-high HDL-C concentrations had a significantly lower risk of Ischemic Heart Disease (IHD) than those with low LDL-C but high TG-low HDL-C concentrations. The major new finding from this study was that men with major classic risk factors of IHD such as a high LDL-C level, hypertension, low physical activity, and smoking still had a low risk of IHD if they had low TG–high HDL-C concentrations. In addition, the results showed that a high TG–low HDL-C concentration was a stronger risk factor than several major conventional risk factors of IHD, such as a high LDL-C.
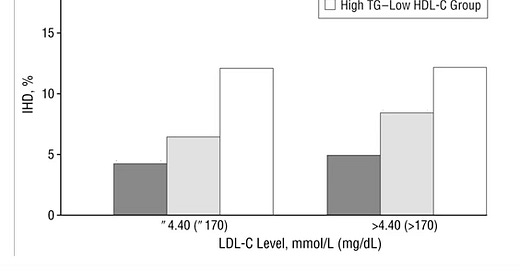
The above figure shows the impact of TG/HDL-C ratio on the IHD incidence stratified by LDL-C level (≤170 mg/dL or >170 mg/dL]. It is clear that those with a high LDL-C level and a low TG/HDL-C ratio had a significantly lower risk of IHD than those with a low LDL-C level and a high TG/HDL-C ratio. In fact, the IHD incidence of the “High TG-Low HDL-C Group” with a low LDL-C is approximately 2 to 3 times higher than that of the “Low TG-High HDL-C Group” with high LDL-C.
The TG/HDL ratio is closely linked to insulin resistance and is considered a marker for metabolic syndrome1. Studies have shown that the TG/HDL-C ratio is more closely associated with the development of insulin resistance than either triglycerides or HDL alone. It is considered a straightforward quantifiable measurement of insulin resistance and a marker of diabetes and coronary heart disease.
Research has also demonstrated that the TG/HDL-C ratio is a strong predictor of obstructive coronary artery disease. In patients with stable angina2, a higher TG/HDL-C ratio (>3.38) was associated with an almost twofold increase in the risk of non-fatal heart attack and all-cause death. In these patients, the TG/HDL-C ratio progressed over time despite increased use of lipid-lowering drugs and reduction in LDL-C. In patients with stable angina, high TG and low HDL-C levels are associated with poor coronary artery disease related outcomes independently of LDL-C and treatments.
The strong focus on LDL-C has overshadowed the importance of the TG/HDL-C ratio. A high LDL-C level with a low TG/HDL-C ratio typically indicates isolated hypercholesterolemia3, which doesn’t necessarily signal high risk for heart disease. In contrast, a high TG/HDL-C ratio often signals metabolic syndrome, involving issues like insulin resistance, glucose intolerance, and hypertension. This ratio also influences LDL particle size, leading to smaller, denser, more oxidation-prone particles that increase plaque risk. High LDL-C without a high TG/HDL-C ratio generally produces larger, less plaque-forming LDL particles, not commonly linked to metabolic syndrome. (I will cover the effect of LDL particle size on coronary heart disease risk in a subsequent post).
Concerning drug treatment, results suggest that persons with hypercholesterolemia and low TG–high HDL-C levels probably do not require drug treatment of hypercholesterolemia but only dietary advice because their absolute risk of IHD is low, a finding in accordance with the West of Scotland Coronary Prevention Study. Results have also suggested that fibric acid derivatives might be useful in people with high LDL-C levels and high TG–low HDL-C levels and that statins might be useful in lowering the risk of IHD in people with high TG–low HDL-C levels. To improve the TG/HDL ratio, reducing triglycerides is essential. Dr. Lustig advises that the best way to lower triglycerides is by cutting back on sugar and carbohydrates. He also recommends avoiding high-glycemic foods, which can spike blood glucose and are often converted into triglycerides. Boosting HDL is the other key factor in improving this ratio. Increasing HDL can be achieved through regular exercise and consuming healthy fats.
Takeaway: In conclusion, the TG/HDL-C ratio is considered a valuable biomarker for cardiovascular health due to its strong associations with insulin resistance, metabolic syndrome, coronary artery disease, and cardiovascular events. Its ability to capture a specific atherogenic lipid profile and its practical clinical utility make it a useful tool for risk assessment and potentially for guiding preventive strategies. Particularly noteworthy is the evidence that individuals with high LDL-C but favorable TG/HDL-C ratios may have lower cardiovascular risk than those with the opposite profile, highlighting the importance of considering this ratio in risk assessment.
Metabolic syndrome is a group of risk factors that increase the likelihood of developing heart disease, stroke, and type 2 diabetes.
Stable angina is characterized by chest discomfort that is provoked with exertion and alleviated at rest or with nitroglycerin. This is often one of the first manifestations or warning signs of underlying coronary disease.
Refers to high levels of cholesterol in the blood.



Good one Ram and no question TGs are bonafide "residual risk" for CVD i.e., even if LDL (in all forms) is controlled, high TG will lead to a higher CVD risk. We are entering a new ear of TG control with drugs in development now - Olezarsen, Volanesorsen; both targeting ApoC-III and a different one targeting ANGPTL3. It will be interesting to see how any or all of them reduce "residual risk" for TGs in the real world. OTOH, there has been much lower success with drugs trying to increase HDL. When it comes to the ratio, it appears we have more control over combating the numerator than denominator at least from a drug treatment perspective. Of course, diet and lifestyle changes should still be the 1st choice to decrease TG and increase HDL.
Here is a fun fact - dogs have a high HDL and lower leves of other TRL (triglyceride rich lipoproteins) so they tend to be resistant to atherosclerosis. Somewhere back in the evolutionary story, we humans seem to have missed out on this trick.... a story similar to loss of uricase. Too bad, there is no return policy ;-)