Making Sense of Your Lipid Panel: Cracking the Code
Understanding LDL, HDL, Triglycerides, and the Alphabet Soup of Cholesterol Markers
LDL, HDL, non-HDL, Lp(a), triglycerides... they all pop up on your lipid panel report like alphabet soup. But what do they actually mean? Let’s break it down in this post and make sense of these biomarkers.
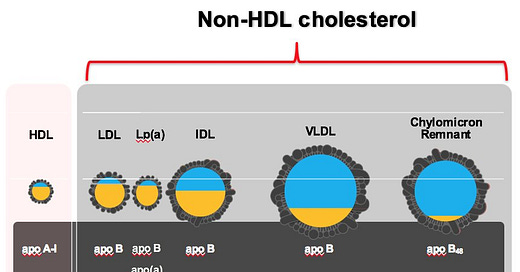
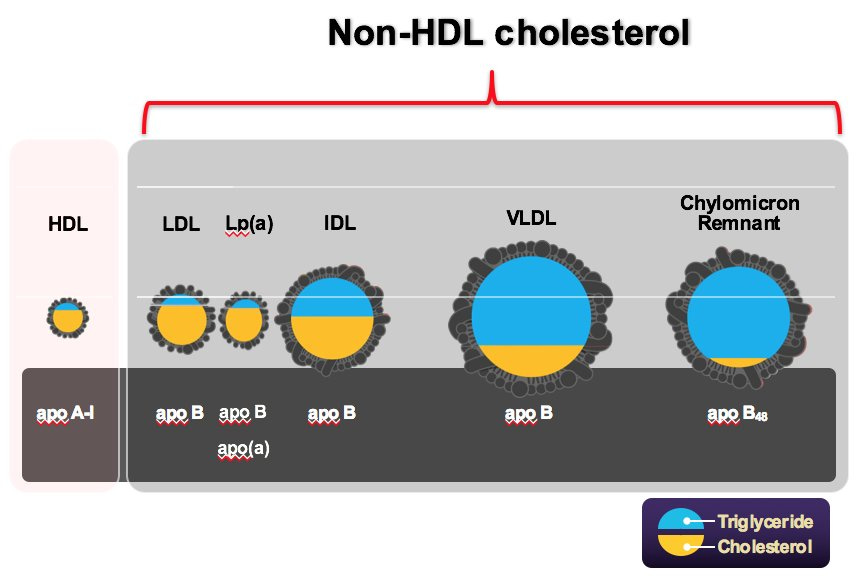
Most of us are aware that our blood transports both cholesterol and triglycerides. But how is it transported? The accompanying figure shows a detailed breakdown of the various lipoprotein particles found in our blood:
Low-Density Lipoprotein (LDL) particles: Often called "bad" cholesterol, it is the primary carrier of cholesterol in the blood. LDL particles make up about 70% of circulating apolipoprotein B (apoB) - containing particles
Very-Low-Density Lipoprotein (VLDL) particles: are the primary carrier of triglycerides synthesized by the liver to peripheral tissues and larger than LDL particles.
Intermediate-Density Lipoprotein (IDL) particles: carry both cholesterol and triglycerides, and is the transitional form between VLDL and LDL.
Lipoprotein(a) [Lp(a)]: A variant of LDL that includes apolipoprotein(a) [apo(a)]. There is an entire post devoted to this particle, that is associated with increased cardiovascular risk.
Chylomicrons: constitute the largest lipoprotein particles and transport dietary triglycerides from the intestines to the other parts of the body, and hence present in blood after meals.
Chylomicron Remnants: are formed after chylomicrons deliver triglycerides to tissues.
High-Density Lipoprotein (HDL) Particles: Often called "good" cholesterol, which help remove excess cholesterol from the bloodstream, and transports it back to the liver for disposal. They are smaller and more abundant than LDL particles, making up over 90% of all lipoprotein particles in circulation.
As shown in the figure, all lipoproteins transport both triglycerides and cholesterol, but the proportion varies significantly among the different types. Chylomicrons and VLDL are primarily responsible for triglyceride transport, while LDL is the main carrier of cholesterol. HDL plays a crucial role in reverse cholesterol transport, helping to remove excess cholesterol from tissues. All non-HDL particles (LDL, VLDL, IDL, Lp(a)) carry apoB and make up less than 10% of total particle number, and are considered atherogenic1. HDL particles are markedly smaller and far more abundant, accounting for over 90% of all particles. They also do not contain apoB and are not considered atherogenic. Cholesterol can only enter the arterial wall through apoB-containing particles. The number of apoB particles that enter and become trapped in the arterial wall is a primary determinant of atherosclerosis risk. According to Peter Attia, apoB is considered a more accurate marker of cardiovascular risk than LDL-C, because each atherogenic lipoprotein particle, such as LDL, VLDL, and IDL, contains one molecule of apoB. Therefore, measuring apoB provides a direct count of the number of atherogenic particles in the blood, which is crucial for assessing cardiovascular risk.
It follows then that LDL particles do not completely convey the risk of plaque accumulation. Non-HDL cholesterol is a true marker of atherogenic risk because it captures all potentially atherogenic particles. This distinction is fundamental to our understanding of lipid-related cardiovascular risk.
High Triglycerides Are An Independent Risk Factor Even With Normal Lipid Levels
Triglycerides play a crucial role in the body as they serve as the primary form of energy storage, that is utilized when the body requires it, such as during fasting or physical exertion. As described earlier, triglycerides are transported in the blood via chylomicrons, VLDL, and IDL, to be delivered to tissues when they are needed, such as during fasting or physical activity. While triglycerides are vital for energy storage and metabolism, maintaining them within a healthy range is essential to minimize the risk of cardiovascular diseases and other health complications. High triglyceride or Hypertriglyceridemia can contribute to the hardening or thickening of artery walls (atherosclerosis), which can lead to cardiovascular events. In addition to genetic reasons, regularly consuming more calories than the body needs, particularly from simple and refined carbohydrates and unhealthy fats, leads to elevated triglyceride levels.
In addition to an unhealthy diet, lack of exercise can contribute to higher triglyceride levels, as exercise helps burn excess calories and improve lipid metabolism. Drinking excessive amounts of alcohol is another major contributing factor, as alcohol is metabolized into triglycerides in the liver. Attached is a table that describes normal and abnormal levels of triglycerides and their impact on health:
Note: Be sure to fast before having your triglyceride levels measured.
Recommendations for Triglyceride Levels ≥ 500 mg/dL
When triglyceride levels are higher than 500 mg/dL, it is generally recommended to consider medication to manage the condition and reduce the risk of complications such as pancreatitis.
Medication: This study found that significant, dose-dependent reductions in triglycerides (22-45%) were observed in subjects with baseline triglyceride levels greater than 250 mg/dL. The study also highlighted that the triglyceride-lowering effect of statins is dose-dependent. Higher doses of statins, such as atorvastatin and simvastatin, were associated with larger reductions in triglyceride level. Statins lower triglyceride levels by reducing the production of VLDL in the liver, which is a major carrier of triglycerides in the blood as discussed previously. This reduction in VLDL leads to decreased triglyceride levels in the bloodstream. In addition, fibrates are often prescribed to reduce triglyceride levels and are considered a first-line treatment for patients with very high triglycerides (≥500 mg/dL) to lower the risk of pancreatitis. Prescription-strength omega-3 fatty acids can also be used to lower triglycerides. These are particularly effective in combination with other lipid-lowering therapies.
Lifestyle Modifications: A very low-fat diet is recommended, especially if triglyceride levels are extremely high (≥1000 mg/dL). Patients should avoid alcohol and refined carbohydrates.
Risk of Pancreatitis: Elevated triglyceride levels, particularly those above 1000 mg/dL, significantly increase the risk of acute pancreatitis (which is a condition characterized by the sudden inflammation of the pancreas). It can lead to complications such as kidney failure, breathing problems, infections, and the formation of fluid-filled sacs. Therefore, aggressive management of triglyceride levels is crucial to prevent this serious complication.
Recent evidence suggests that high triglycerides are an independent risk factor for cardiovascular disease, even when other lipid levels are normal. A large-scale study published in the Journal of the American College of Cardiology in 2022 found that elevated triglycerides were robustly associated with an increased risk of atherosclerotic cardiovascular disease (ASCVD), independent of LDL-C levels. This study, which included over 68,000 individuals, demonstrated that high triglycerides were associated with increased risk even when LDL-C levels were normal. In addition, the PESA (Progression of Early Subclinical Atherosclerosis) study highlights the importance of considering triglyceride levels in cardiovascular risk assessments, even when LDL-C levels are normal, due to the independent risk posed by elevated triglycerides.
Takeaway: Look at the non-HDL cholesterol number in your lipid profile — not just LDL-C. The former is a true marker of atherogenic risk because it captures all potentially atherogenic particles. High triglycerides are a serious risk factor on their own, independent of LDL values. If your levels are above 200, talk to your doctor as soon as possible.
tending to promote the formation of fatty plaques in the arteries.




Great article. A topic of interest for most people.
Excellent article!! Easy to read