Decoding the Glucose Rollercoaster: My CGM Adventure
From Morning Workout Spikes to Cookie vs. Kale Showdowns: Unveiling Hidden Health Insights with Continuous Glucose Monitoring
In a previous post, I explored how Glucose Variability (GV) offers deeper insights into risks like insulin resistance and cardiovascular health—insights you just can’t get from average glucose metrics like fasting glucose or A1c. I also highlighted how Continuous Glucose Monitors (CGMs) can be a game-changer, giving you real-time updates on your blood sugar levels. I also promised to document my experience with CGMs, so here it is.
How Does a CGM Work?
A CGM works by measuring glucose levels in the interstitial fluid1 between cells, which closely correlates with blood glucose levels. A tiny sensor (small needle) is inserted under the skin, usually under the arm. The sensor uses enzymatic technology to react with glucose molecules, generating an electric current proportional to glucose concentration. A transmitter attached to the sensor wirelessly sends data to a smartphone. The receiver displays glucose readings, typically updating every 1 to 15 minutes.
Modern CGMs are quite accurate, with some achieving a mean absolute relative difference (MARD)2 as low as 7.9%. CGMs may be less accurate during rapid glucose changes, such as after meals or during exercise. There is a physiological delay between changes in blood glucose and interstitial fluid glucose, which is typically around 5-15 minutes. The delay can be more pronounced during rapid glucose fluctuations, such as during exercise or in the postabsorptive state3.
I chose the FreeStyle Libre 3 system for my CGM journey. It features the world’s smallest and thinnest glucose sensor (as shown below) —just 2.9 mm high and 21 mm in diameter. With real-time glucose readings every minute, it streams data directly to my iPhone, eliminating the need for manual scanning. It’s also the most accurate CGM on the market, boasting a MARD of 7.9%. No fingerstick calibrations are needed, and it offers customizable alarms for high and low glucose levels, with a 14-day wear time. Plus, it’s water-resistant up to 3 feet for 30 minutes and can be worn during showers, which is pretty convenient. The sensor's range is about 35 feet, and it keeps you informed with alerts when you step out of range from your iPhone. If you’re not diabetic, your insurance likely won’t cover the FreeStyle Libre device. I paid around $80 for a single sensor (using a GoodRx discount), which lasts about two weeks. Implanting4 and activating the sensor was quick and straightforward.
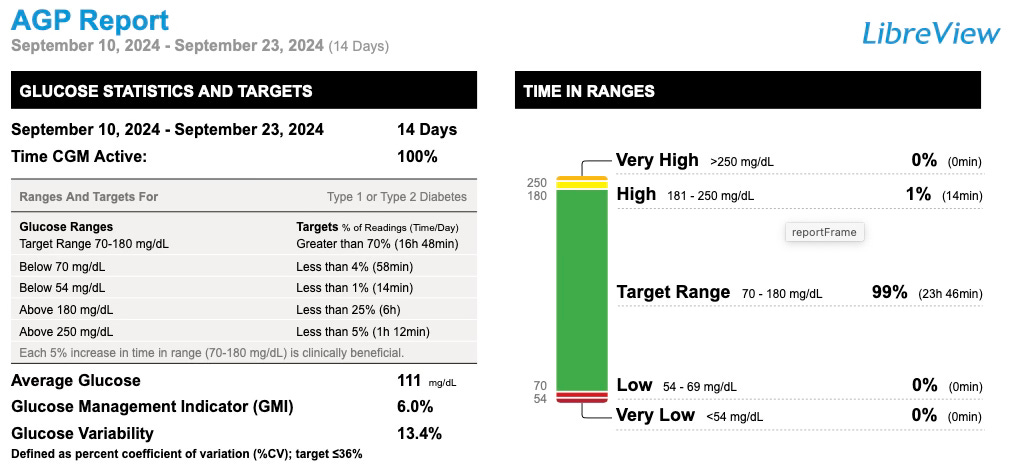
The FreeStyle Libre CGM also has a cloud-based portal, LibreView that provides detailed insights into the user’s glucose variability. Specifically, there are two key graphs that are quite useful:
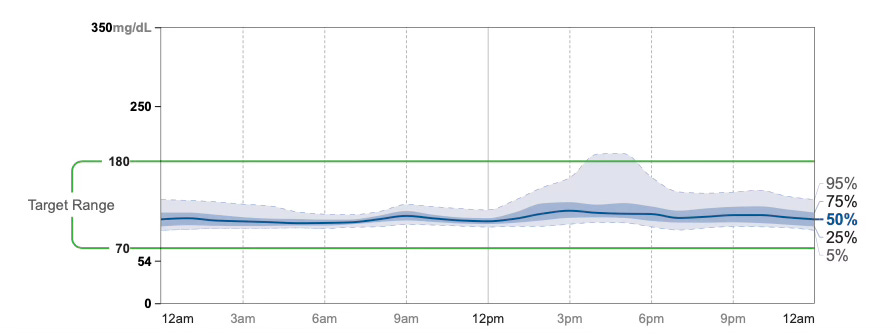
Ambulatory Glucose Profile (AGP): (as shown below) is a visual summary of glucose trends over a typical day, aggregating data over 14 days to highlight patterns and fluctuations. It helps identify consistent high or low glucose periods and overall variability.
Time-in-Range Report: shows the percentage of time my glucose levels stayed within a target range, emphasizing stability over spikes or prolonged lows. It is worth noting that I intentionally tested the impact of alcohol, processed foods, and high-sugar foods on my glucose variability. Thankfully, my usual dietary choices generally keep my glucose levels from hitting those “high” values.
There are also daily graphs, which display day-by-day glucose readings, showing real-time spikes, dips, and their timing. One can correlate these trends with activities like meals or exercise.
The Glucose Puzzle: Why Morning Workouts Cause a Sugar Surge
In an earlier post, I shared my experience with intermittent fasting, where I start eating at noon. My mornings begin with exercise between 8 and 9 AM. As shown in the charts, my glucose levels are around 100 mg/dL before my workout but spike up to 140 mg/dL during exercise. I was quite surprised by this spike in glucose.


It turns out that this temporary elevation in glucose levels has multiple reasons:
Hepatic glucose production: During fasting and high-intensity exercise, the liver increases glucose production to maintain blood glucose levels. This process, known as gluconeogenesis, is enhanced in the absence of recent food intake.
Stress hormone response: High-intensity exercise, such as high-intensity interval training (HIIT), triggers the release of stress hormones, particularly adrenaline, which stimulates the liver to release glucose into the bloodstream. This hormonal response is more pronounced during fasting and high-intensity exercise.
Cortisol levels: Fasting morning exercise is associated with higher plasma cortisol levels, which tend to be higher in the morning than in the afternoon. Elevated cortisol can contribute to increased glucose production and reduced insulin sensitivity.
Cookies vs. Kale: A Tale of Glucose Spikes and Health Insights
One of the reasons for my CGM journey was to compare the effects of a low-carb, veggie-rich diet with those of a high-sugar diet on blood glucose levels. In a previous post about glucose variability, I explained why sharp spikes in blood sugar and insulin are more harmful than a steady, moderate rise. Research underscores this concern, showing that post-meal glucose spikes can be particularly damaging to cardiovascular health.
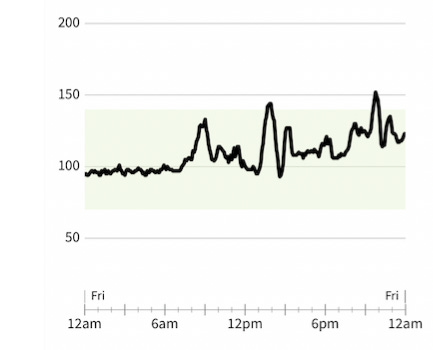
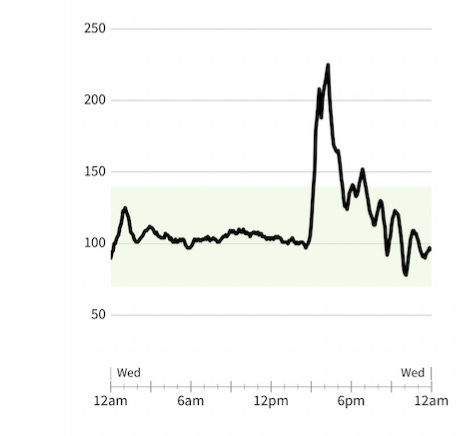
The pictures say it all! The left panel captures my glucose variability after breaking my intermittent fast at noon with a meal rich in veggies, tofu, fruit, and a modest amount of carbs (the 8 AM spike reflects my earlier morning workout). In sharp contrast, the right panel showcases the dramatic glucose surge that followed breaking my fast with two oversized sugar cookies. The difference is as clear as cookies vs. kale! Even though I consumed fewer calories in the second case, the sugar-fueled spike and increased variability are much more damaging to my metabolic health. It is a clear example of how food choices impact glucose control beyond just calorie counts. A sharp-eyed reader might notice the glucose spike in the early morning hours on the right panel. This likely resulted from my alcohol consumption the night before. The concerning part? After a night of drinking, glucose levels never fully stabilize, which has potentially risky implications for metabolic health. Clearly, alcohol disrupts normal glucose regulation and its effects on blood sugar can persist well into the next day.
It is well known that glucose spikes activate inflammatory processes that contribute to long-term vascular damage. Research also indicates that glucose variability, rather than just average glucose levels, is an important factor in diabetes complications.
Takeaway: CGMs reveal how diet, exercise, and habits like alcohol consumption impact glucose variability. By analyzing real-time data through tools like the Ambulatory Glucose Profile (AGP) and Time-in-Range reports, I uncovered how factors like morning workouts and sugary snacks create dramatic glucose spikes. The findings highlight the importance of consistent dietary choices for metabolic health and the hidden dangers of glucose fluctuations triggered by alcohol or high-sugar foods.
Interstitial fluid is a fluid that surrounds cells and tissues in the body, carrying nutrients and waste products. It's similar in composition to plasma, but has lower concentrations of proteins.
MARD is the average difference between a CGM's measurement and a reference measurement, expressed as a percentage. A lower MARD indicates better agreement between the CGM and the reference measurement. MARD is often used to assess the accuracy of continuous glucose monitoring (CGM) systems
The postabsorptive state, also known as the fasting state, is the metabolic state that occurs after digestion when the body is no longer getting nutrients from food. It typically happens overnight, but fasting during the day can also put the body in this state. During this state, the liver generates ketones for use by other tissues.
The sensor has a tiny, flexible filament which feels like a quick pinch, when inserted into the skin.





OTC CGMs are powerful tools for providing real-time biofeedback that can motivate behavior changes. I would recommend a CGM trial for anyone whose A1c has been trending upward.