Inflamm-aging Uncovered: Chronic Inflammation and Its Hidden Impact on Health
How CRP Levels Reveal the Silent Fire Driving Aging and Chronic Disease
“Inflamm-aging” is the hot new buzzword lighting up health headlines, and for good reason—it links chronic low-level inflammation to aging and age-related diseases. Inflamm-aging is like your immune system constantly buzzing with tiny inflammations that never fully calm down. It’s the biological equivalent of leaving all your devices on standby; they’re not off, but they’re draining energy and causing wear. This chronic inflammation accelerates your biological clock, making your cells and body age faster than the latter’s chronological age. Chronic inflammation is linked to nearly every major chronic disease: heart disease, cancer, diabetes, high blood pressure, Alzheimer’s, depression, autism, autoimmune diseases, allergies, asthma, and aging itself.
Chronic Inflammation: What Is It and How to Track It?
Inflammation is part of the body’s defense system. We are all familiar with inflammation that results from a sore throat or sprained ankle. The classic signs of inflammation are pain, swelling, redness, and heat. This is the body’s acute response to infection or injury. Once the insult or injury is resolved, the inflammation subsides. However, research over the last 30 years has found that low-level chronic inflammation, which is not related to injury or infection, is the major driver of chronic disease and aging. It is silent and has no symptoms but acts as a disease accelerating smoldering fire inside your body. Chronic inflammation is often referred to as the “silent killer.” This inflammation accelerates heart disease, diabetes, cancer and dementia.
The primary driver of chronic inflammation is our ultra-processed, high-sugar, high-starch diet, which promotes inflammation via mechanisms like visceral fat accumulation. These fat cells release inflammatory cytokines, contributing to obesity-related diseases like heart disease, diabetes, cancer, and dementia. Additionally, this diet disrupts the gut microbiome, leading to a “leaky gut” where bacterial toxins and food particles pass through the gut lining, activating the immune system and fueling systemic inflammation. Other triggers include environmental toxins (e.g., pesticides, heavy metals), food sensitivities, allergies, and stress—both physical and psychological—all of which exacerbate inflammation.
The most common test for assessing inflammation is high-sensitivity C-reactive protein (hs-CRP), a measure of one of the body’s immune messengers called cytokines. hs-CRP is a protein produced in the liver and released into the blood in response to various triggers such as viral or bacterial infection, injury, or other chronic conditions such as an inflammatory diet, sedentary lifestyle, chronic stress, toxins, allergens, or dysbiosis (imbalances in your gut flora or microbiome). It is also linked to mental illness and autism. CRP testing is still uncommon, so request your clinician to add it to your panel at your next physical, especially if you are concerned with your cardiovascular health. CRP is directly involved in vascular pathology through the activation of inflammatory cells, caused by oxidative stress. Oxidative stress1 activates immune cells such as macrophages, neutrophils, and monocytes2, releasing pro-inflammatory molecules, further propagating the inflammatory response.
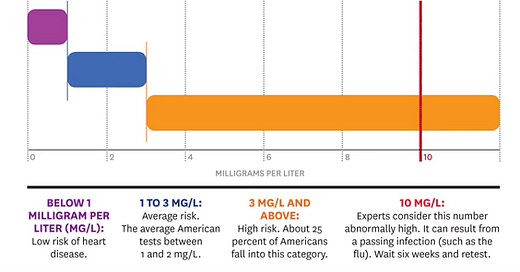
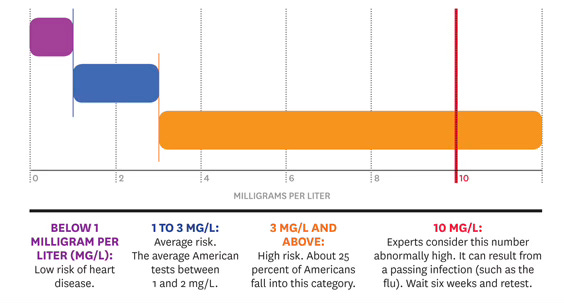
CRP levels can increase with age, but normal ranges vary by lab. In general, a normal CRP level is less than 0.9 milligrams per deciliter (mg/dL). Higher CRP levels correspond to higher risk of heart disease as shown in the chart below.
Healthy CRP levels vary by age and sex. The following formulas provide approximate healthy upper reference limits for CRP levels for adults aged 25-70 years:
Men: CRP (mg/dL) = age/50
Women: CRP (mg/dL) = age/50 + 0.6
For example, a 50-year-old man would have a healthy upper limit of 1.0 mg/dL, while a 50-year-old woman would have a healthy upper limit of 1.6 mg/dL. It's important to note that these are upper reference limits, and lower levels are generally considered healthier.
High CRP Levels Lead to Poor Disease Outcomes
A study of ICU patients found that elevated CRP concentrations on admission were correlated with an increased risk of organ failure and death. Patients with CRP levels >10 mg/dL had significantly higher incidence of respiratory, renal, and coagulation failures, as well as higher mortality rates compared to those with CRP <1 mg/dL. For instance, in COVID-19 patients, higher CRP levels were associated with increased mortality risk. A retrospective cohort study of 3,545 patients found that mortality rates increased from 11.94% in the lowest CRP tertile to 41.33% in the highest CRP tertile. Finally, in cardiovascular diseases, elevated CRP levels have been shown to predict adverse cardiovascular events and are associated with increased risk of future cardiovascular events. Studies show that higher CRP levels are linked to worse outcomes and higher mortality in conditions like critical illness, COVID-19, stroke, and cardiovascular disease, underscoring CRP's value as a predictor of disease severity. Elevated CRP is also common in metabolic syndrome, which includes insulin resistance, obesity, dyslipidemia, and hypertension. Research reveals that high CRP levels are associated with a greater risk of diabetes, dyslipidemia, and metabolic syndrome, highlighting chronic low-grade inflammation as a key feature of both metabolic syndrome and type 2 diabetes.
Statins: Reduces CRP in Addition to Cholesterol Control
Traditional medications like anti-inflammatories, steroids, and immunosuppressants fail to address the root causes of chronic inflammation. These drugs may ease symptoms of autoimmune diseases or allergies but don't resolve the underlying problem. However, several studies have consistently demonstrated that regular statin use leads to significant reduction in CRP levels, highlighting its anti-inflammatory effects beyond lipid-lowering properties. A large network meta-analysis of 37 randomized controlled trials with 17,410 participants found that statins significantly decreased CRP levels compared to controls. A study on simvastatin found that it lowered highly sensitive CRP (hsCRP) levels within 14 days of initiation, independent of its effect on LDL cholesterol. Median hsCRP decreased from 2.55 mg/L at day 0 to 1.60 mg/L at day 14 for patients on simvastatin, compared to 2.00 mg/L and 2.20 mg/L at days 0 and 14 for patients on placebo. Research has shown that statins can reduce CRP levels by up to 60%, with this effect being independent of LDL cholesterol lowering. In patients with acute coronary syndromes, both atorvastatin and pravastatin were found to significantly lower CRP levels, with atorvastatin showing a more pronounced effect.
In conclusion, CRP is a versatile biomarker that offers valuable information about systemic inflammation, metabolic health, and overall biological well-being. Its levels can help identify individuals at risk for various chronic diseases and guide preventive strategies and treatments.
Takeaway: CRP is a key biomarker of chronic low-grade inflammation, linked to aging and major diseases like heart disease, diabetes, and dementia. Elevated CRP often results from poor diet, stress, toxins, and gut imbalances. CRP testing is still uncommon, so request it at your next physical. Statins can lower CRP, offering anti-inflammatory benefits beyond cholesterol control.
Oxidative stress occurs when there is an imbalance between free radicals and antioxidants in the body. Excess free radicals damages cellular components, which triggers an inflammatory response.
All are immune cells that protect your body: Macrophages: Large cells that "eat" pathogens and debris, Neutrophils: First responders that attack infections, and Monocytes: patrol blood for threats.



A timely topic Ram, particularly since I suspect there is a general lack of awareness on the contribution of inflamm-aging to senescence. As with any 'new' therapeutic opportunity, there has been some progress in a few areas, however, apart from say diet and exercise, I think drug trials are still in early stages despite some successes. Another challenge is the multifactorial nature of this beast - right from choosing appropriate molecular targets to figuring our primary and seconday enpoints for regulatory studies for approval, there is lot of work to be done so to speak. One hopes there will be continued support for basic research in this area for it is likely to be exploratory more towards generating hypothesis that can be tested in future be it specific/targeted diet or lifestyle factors or even therapeutic interventions.