Rethinking Stress Tests: Are They Overrated in Heart Disease Diagnosis?
Why Modern Imaging Tools like CCTA and CAC Scoring Are Outpacing Traditional Exercise Tests
A few years ago, while returning to the airport from a business trip to Ann Arbor, Michigan, I experienced mild chest pains and a throbbing sensation in my left arm. Not wanting to take any chances, my colleague urged me to visit a nearby hospital rather than board my flight. I ended up spending the night in the emergency ward and undergoing an exercise stress test the next day, which came back negative. It turns out that it was not a good use of time and money. The stress test, often seen as a cornerstone of diagnostic cardiology, is widely recognized by both doctors and patients. However, both groups have been misguided in their understanding and use of it. The famed “Meet the Press” anchor, Tim Russert passed an exercise stress test just 2 months prior to his Sudden Cardiac Death (SCD). Based on his autopsy results this is not surprising, because he did not have significant coronary stenosis1 other than the one lesion that acutely thrombosed2 at the time of his SCD. Clearly, stress tests cannot predict short-term risk of heart attacks or death.
An exercise stress test is used to evaluate how well your heart functions during physical activity. It measures your heart's response to exercise by monitoring its electrical activity, heart rate, blood pressure, and oxygen consumption. During the test, you typically walk on a treadmill or pedal a stationary bicycle while connected to an electrocardiogram (ECG) machine. The exercise intensity gradually increases, usually every three minutes, by adjusting the speed and incline of the treadmill or the resistance on the bike. Throughout the test, medical professionals closely monitor your vital signs and ECG readings. The test continues until you reach your target heart rate, develop concerning symptoms, or become too fatigued to continue. Exercise stress tests are used by healthcare providers to diagnose coronary artery disease, and assess the severity of heart conditions.
The main problem with this procedure is that it is just not an effective diagnostic tool. Numerous studies have shown that exercise stress testing has a relatively low sensitivity for detecting mild to moderate coronary artery disease (CAD):
Insufficient Ischemia: Exercise stress testing may not induce enough myocardial ischemia3 to be detected in patients with mild to moderate coronary artery stenosis. This is particularly true for cases where there is less than 50% stenoses.
Dynamic Nature of CAD: The test captures a snapshot in time, but CAD is a dynamic process. Plaques that don't cause significant stenosis during the test may still rupture and cause acute coronary events later.
Submaximal Exercise: Some patients may not achieve maximal exercise capacity, reducing the test's ability to induce detectable ischemia. This actually happened in my case and the attending clinician chose to stop the test.
Single-Vessel Disease: The sensitivity is lower in patients with single-vessel disease compared to multi-vessel disease (This is exactly what happened with Tim Russert).
Gender and Age Differences: The test has lower sensitivity in women, particularly during their reproductive years due to hormonal influences. In younger patients (under 40), the incidence of positive findings is very low (0.4%), further reducing the test's overall sensitivity.
A high-quality study found that stress tests had a sensitivity of only 45% for detecting coronary stenosis, which is worse than chance. It also suffers from a poor predictive value for cardiac events. In a large study of over 25,000 men followed for nearly 10 years, 40% of those who suffered cardiac death had completely normal stress test results. Of course, the most important metric for any health care measure is also the simplest: does it help people? Perhaps the most definitive and most important recent study of stress test screening is the ‘DIAD’ trial, published this year in the Journal of the American Medical Association. The trial randomized diabetics (mean age 61) without known coronary disease, a group considered to be high risk, to either have or not to have a nuclear stress test4 at baseline. After 5 years an identical number of subjects in each arm of the study had suffered heart attacks or death. In other words, being screened for heart disease with a nuclear stress test (ostensibly the most accurate type of stress test) did not reduce cardiac events or deaths—the tests didn’t help people.
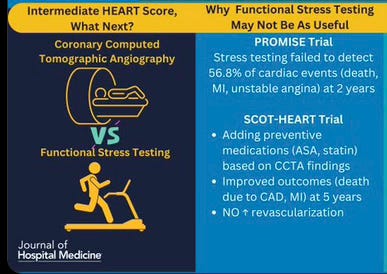
These findings suggest that stress tests may not be as effective as previously thought in diagnosing CAD or predicting cardiac events. As mentioned in my previous posts, there is significant evidence that Coronary artery calcium (CAC) scoring and Cardiac CT Angiography (CCTA) offer several advantages over exercise stress testing and nuclear stress testing for diagnosing CAD.
CCTA consistently demonstrates higher sensitivity compared to stress testing methods. In a meta-analysis of 11 studies with 1,575 patients, CCTA showed a pooled sensitivity of 98% vs. 67% for exercise stress test. As discussed in my earlier post, CCTA can visualize both calcified and non-calcified plaque, as well as assess the severity of stenosis, providing a more complete picture of coronary health. CAC scoring has shown high sensitivity (98%) for predicting significant coronary stenosis.
In addition to serving as a better diagnostic tool compared to stress testing, CCTA has a higher clinical impact. The SCOT-HEART study showed that CCTA resulted in reclassification of CAD diagnosis in 27% of patients vs. 1% in the standard care group, leading to changes in preventative measures. Several studies have shown trends towards lower cardiac event rates with CCTA-guided management compared to the traditional approach with stress testing. Use of CCTA and CAC scoring also leads to higher use of medications such as aspirin and lipid-lowering agents such as statins compared to stress tests.
When is stress testing most useful? While CCTA and calcium scoring often provide superior diagnostic performance, stress testing is more effective in specific scenarios. For example, it is recommended for patients with high CAC scores (>400), as elevated calcium levels can interfere with lumen visualization during CCTA. Stress testing is also valuable for identifying high-risk patients who may benefit from revascularization5 and for monitoring responses to medical or surgical interventions in cases of valve disease, arrhythmias, or other heart conditions. In summary, stress testing remains essential for functional assessment and identifying high-risk patients. The choice between these methods should depend on the clinical context and individual patient needs.
Takeaway: Exercise stress tests, once a cornerstone of cardiac diagnostics, are facing scrutiny due to their low sensitivity in detecting coronary artery disease and limited predictive value for cardiac events. Modern alternatives like CCTA and CAC scoring are emerging as superior options, offering higher accuracy and greater clinical impact. However, stress testing still holds value in specific scenarios, such as assessing patients with high calcium scores or monitoring post-intervention recovery.
Stenosis is a narrowing of any passageway in the body that prevents a substance or structure from passing through easily. It can occur in many parts of the body, including blood vessels, heart valves, and respiratory system.
Thrombosed means affected by a blood clot, or thrombus, that blocks an artery or vein. Thrombosis is a serious medical condition that can lead to life-threatening complications like stroke or heart attack.
Myocardial ischemia, also known as cardiac ischemia, is a condition that occurs when the heart muscle doesn't receive enough oxygen due to reduced blood flow. This happens when the heart's arteries, also known as the coronary arteries, are partially or completely blocked.
A nuclear stress test is a type of heart stress test that uses a radioactive tracer injected into the bloodstream to create images of the heart muscle, allowing doctors to see how blood flows to the heart both at rest and during exercise, while a normal exercise stress test only monitors heart rhythm (ECG) changes during physical exertion, without the imaging component; essentially, a nuclear stress test provides a more detailed picture of blood flow to the heart compared to a standard exercise stress test.
Revascularization is a medical procedure that restores blood flow to an organ or body part (mainly heart) that has been affected by ischemia. It can be performed using surgery or minimally-invasive procedures.




If I recall correctly, the last time I think had a stress test was in India when I went for my routine/annual check up and that was over 15 years ago. I have not paid much attention to this one but based on your research, it appears it may still be useful for identifying high risk patients? If so, I guess you are still looking at a subset of patients who have not had any major 'event' to date or otherwise blissfully unaware of their risk category? Is this interpretation correct?