Beyond Annual Checkups: Why Regular Biomarker Testing is the Future of Preventive Health
We track our steps and sleep daily—so why are we still relying on once-a-year health checkups? A deep dive into Function Health’s approach to early disease detection and proactive health monitoring.
It is pretty remarkable how we have embraced daily health tracking—counting steps, monitoring heart rate, and analyzing sleep with smart devices. Yet, when it comes to crucial health biomarkers, we still rely on infrequent annual check-ups. As we age, our bodies change, and the risk of chronic disease rises, making regular biomarker monitoring even more essential. More frequent testing can help detect metabolic shifts early, allowing for timely interventions and better long-term health. Dr. Casey Means, author of Good Energy, argues that the typical annual checkup in the U.S. falls far short of what’s needed for true preventive care. Annual checkups are too infrequent to capture meaningful changes in health status or to provide timely feedback on lifestyle interventions. These checkups happen too infrequently to catch meaningful health changes or provide timely feedback on lifestyle adjustments. Standard tests often overlook key biomarkers that could signal early metabolic issues. For instance, Dr. Means emphasizes the testing of several biomarkers1 such as ApoB (key marker for cardiovascular health), Lp(a) (a type of fat in the blood that increases the risk of heart disease), and hs-CRP (a key marker of chronic inflammation) that are not typically included in standard annual checkups. Like Dr. Peter Attia, she also criticizes the healthcare system for focusing more on treating diseases after they appear rather than preventing them in the first place.
After a Calcium CT scan revealed calcified plaque in my arteries, I was prescribed statins, which made me more vigilant about monitoring my health. Since then, I have made it a priority to check my lipid profile and HbA1c every six months. So far, I have been using Ulta Labs, which offers a range of discounted health screenings. However, the costs add up quickly—a comprehensive lipid panel alone is $131, while tests for hs-CRP ($34), PSA ($53), and glucose ($28) bring the total to around $250 for these additional biomarkers.
Enter Function Health, a company that was co-founded by established by Dr. Mark Hyman2, a renowned physician and bestselling author known for his work in functional medicine. Function Health represents a shift in preventive healthcare, offering a more comprehensive and frequent testing approach compared to traditional annual physicals. While standard check-ups typically assess only 20 biomarkers, Function Health reports on 106 biomarkers in its initial assessment, covering areas such as heart health, thyroid function, hormones, and metabolic markers. This testing regime, performed twice a year, allows for early detection of potential health issues and enables individuals to track changes in their health over time. Compared to similar services, Function Health offers a more affordable option with a focus on frequent, comprehensive testing. While other direct-to-consumer lab testing services like Ulta Labs or Life Extension offer individual tests, Function Health's bundled approach provides a more cost-effective and holistic solution for those seeking regular, in-depth health monitoring. Function Health is currently in beta, requiring users to join a waitlist (I was accepted within a few days). For $499 per year, members receive two rounds of testing—an initial assessment covering 105+ biomarkers and a follow-up 3 to 6 months later with 60+ biomarkers to track progress. This allows users to measure the impact of lifestyle changes, such as diet, exercise, or medications, over time. Please feel free to use this link to sign up for their service.
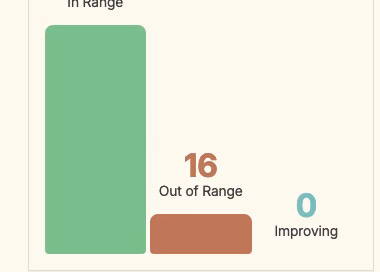
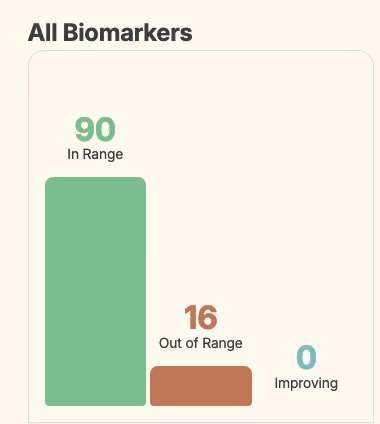
After signing up for the service, I had to visit Quest Diagnostics twice, as Function Health partners with Quest for testing. During these visits, they collected about a dozen vials of blood. Over the next week, my results gradually became available. As shown in the chart, 90 biomarkers were within the normal range, while 16 were outside the expected levels.
Of the 16 markers that were out of range, 10 were related to heart health—which wasn’t surprising. Since starting statins, my LDL-C has dropped to 63 mg/dL, which would typically be reassuring if I were only looking at a standard blood panel, where LDL-C is the primary focus. However, Function Health goes deeper, providing a more detailed breakdown of my LDL profile. In addition to LDL-C, they report on LDL Particle Number, LDL Medium, LDL Small, LDL Pattern and LDL Peak Size, and that’s where the news is not all that great. Rather than just measuring the cholesterol weight (in mg/dL), the lipoprotein fractionation test analyzes the total number of LDL particles that comprise your LDL cholesterol. This test (which accounts for less than 1% of all cholesterol tests, and is therefore most likely not included in your annual blood panel) provides critical insight into the types and numbers of cholesterol particles that comprise a certain weight, such as an LDL of 63 mg/dL. That 63 mg/dL could be comprised of just a few large, fluffy, buoyant LDL particles (good) or hundreds of small, dense, dangerous LDL particles (bad). Think beach ball versus golf ball. Ideally, LDL particle number should be below 1,138, but mine came in at 1,368—so there’s definitely room for improvement. I plan to dive deeper into this topic in a future post, specifically focusing on the lipoprotein fractionation test and what it reveals about heart health. In addition, my Vitamin D levels are lower than ideal, and I also have elevated levels of amylase and lipase—enzymes linked to pancreatic function.
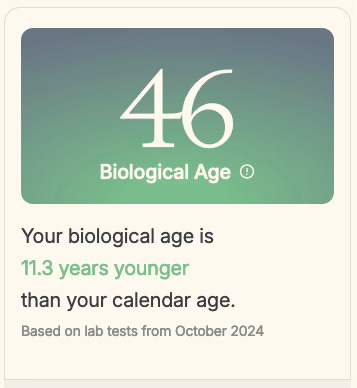
One of the more unconventional health insights I gained was my biological age—which is 46, making me 11.3 years younger than my actual age of 57. This metric reflects how well your body is aging at the genetic, cellular, and molecular levels. When biological age outpaces chronological age, it signals accelerated aging, increasing the risk of conditions like prediabetes, Type 2 diabetes, heart disease, cancer, and hormonal imbalances. While almost every company selling these tests calculates biological age based on a different methodology, Function relies on Phenotypic Age, which is an assessment of biomarkers such as albumin, creatinine, glucose, and mean cell volume. While I was initially skeptical, it turns out the Phenotypic Age calculation appears to have a strong scientific basis, drawing from established research in the field of biological aging.
The calculation involves a linear combination of chronological age and nine clinical biomarkers such as albumin, creatinine, glucose, hs-CRP, lymphocyte percentage, mean cell volume, Red Blood cell distribution Width (RDW), Alkaline phosphatase, and WBC count. Research has shown that Phenotypic Age is a reliable predictor of all-cause and cause-specific mortality in various population subgroups, and the metric can differentiate mortality risk among individuals of the same chronological age. A one-year increase in Phenotypic Age is associated with a 9% increase in the risk of all-cause mortality. The good news is that lifestyle changes can significantly impact Phenotypic Age. Multiple studies have demonstrated that modifiable lifestyle factors can influence biological aging as measured by Phenotypic Age and other epigenetic clocks.
While the lab results were accompanied by pages of personalized clinician notes; what each out-of-range metric meant, and what kind of steps I could take to correct it, like limiting or prioritizing certain foods, and taking supplements. The biggest downside of Function Health is that the clinician’s notes are quite generic and lack specific action steps for addressing out-of-range markers. For example, if a user has multiple abnormal heart health markers, they should be advised to get a Calcium CT scan to assess potential cardiovascular disease. Likewise, someone with an elevated PSA score should be guided toward a more accurate test, like the 4Kscore, to better evaluate the risk of prostate cancer.
Our approach to healthcare is backward—we wait for disease to appear instead of focusing on prevention. I support Function Health’s proactive screening approach to detecting health issues early. I do hope that in the future they provide a clear action plan for addressing the out of range biomarkers.
Takeaway: Most people track daily health metrics like steps and sleep, yet rely on infrequent annual checkups for crucial biomarkers. Function Health aims to change this by offering twice-yearly comprehensive biomarker testing, covering over 100 markers to detect early metabolic shifts and improve long-term health. While its approach enhances preventive care, clearer action steps for addressing abnormal results would make the service even more impactful.
We have written about these biomarkers in detail in prior Substack posts.
In addition to being Function’s chief medical officer, he’s the founder of the Cleveland Clinic Center for Functional Medicine, founder and director of The UltraWellness Center in Lenox, Mass., the author of several bestselling books, and the host of a popular podcast.



I’ve found my results to me enormously helpful with advocating for myself with the limited PCP time and attention.
Highly recommend “The Age of Scientific Wellness” By Lee Hood. It speaks to developing platforms using biomarker data to prevent disease. Lee is a visionary and continues to work towards improving lives at 86 years old.